Women's Health
Hormone Therapy and Personalized Care for Menopause and More!
Peri-Menopause & Menopause Care
At Metrobest Health, we specialize in hormone therapy to help women manage symptoms of menopause, peri-menopause, PCOS, and other hormonal imbalances. Our team provides customized treatment plans to support your health at every stage of life
Hormones in Women: The Foundation of Health
Hormones are chemical messengers produced by specific glands and tissues, traveling through the bloodstream to regulate countless bodily functions and sensations. From childhood to adolescence, adulthood, childbearing years, and menopause, hormone production fluctuates naturally, adapting to each stage of a woman’s life.
However, these hormonal rhythms can be disrupted at any time due to factors like illness, dietary changes, or stress, often leading to health challenges. As women age, ovarian hormone production declines—a natural transition from the childbearing years to menopause. While this is a normal biological process, it’s often associated with negative health outcomes, affecting mental health, cardiovascular health, and bone density.
The Transition of Hormones: Perimenopause
Perimenopause marks a critical hormonal shift before menopause. During this phase, estrogen production begins to decline, resulting in hormonal imbalances that can significantly affect physical and emotional well-being.
Lasting 4 to 8 years, this stage is characterized by irregular menstrual cycles and ends with the final period. One year after the last menstrual period marks menopause, but for many women, the symptoms of perimenopause are at their peak during this transition. Unfortunately, these symptoms are often subtle or mistaken for other health issues, delaying proper diagnosis and care.
COMMON SYMPTOMS OF HORMONAL CHANGES:
Weight Gain and Metabolic Changes
Hormones operate like a symphony, with each playing a crucial role. When estrogen levels drop during perimenopause, the disruption can lead to increased appetite, lower energy, disturbed sleep patterns, and weight gain. Balancing hormones is essential for maintaining metabolic health and achieving weight management goals.
Decline in Libido and Sexual Health
Testosterone and estrogen are vital to maintaining sexual desire and comfort. As testosterone declines, libido diminishes, and lower estrogen levels contribute to vaginal dryness and discomfort during intercourse. Though often seen as a taboo subject, addressing these concerns is critical as they reflect underlying hormonal imbalances.
Depression and Emotional Changes
The link between hormones and mental health is well-documented. Women with a history of depression are at a significantly higher risk of experiencing major depressive episodes during perimenopause. Even those with no prior mental health challenges often report mood swings, anxiety, and depression during this time. Hormonal changes can deeply influence emotional well-being, requiring a proactive and supportive approach.
Loss of Muscle Tone and Strength
Declining estrogen levels lead to cellular dysfunction and increased inflammation, promoting muscle breakdown—a condition known as sarcopenia. This can result in a noticeable loss of muscle tone and strength, highlighting the importance of maintaining a healthy balance of hormones for physical vitality.
Sleep Disturbances
Insomnia is a common concern during perimenopause, with about 50-59% of women reporting sleep difficulties, including nighttime awakenings and trouble staying asleep. Severe hot flashes are strongly linked to chronic insomnia, with over 80% of women experiencing these symptoms also reporting significant sleep disturbances. Addressing hormonal imbalances can improve sleep quality and overall health.
Supporting Hormonal Health
Navigating the hormonal changes throughout a woman’s life requires awareness, understanding, and tailored care. Whether it’s managing symptoms of perimenopause or addressing concerns related to libido, weight, or sleep, balancing hormones is essential for overall well-being. With the right support, women can thrive through every stage of life.
For those facing hormonal changes, we provide personalized menopause care solutions, including lifestyle coaching and hormone replacement therapy. Our approach helps reduce symptoms and supports long-term health.
Hormonal Weight Gain
Our hormone therapy services address various conditions, including menopause care, PCOS management, and andropause.
Hormones and Their Impact on Women's Weight
Hormones play a crucial role in regulating body weight, but they are not the sole factor. Weight gain is influenced by a complex interplay of factors, including diet, physical activity, genetics, and medications. However, hormones significantly affect appetite, metabolism, and fat storage.
KEY HORMONES AFFECTING WEIGHT
Insulin: The Blood Sugar Regulator
Insulin, a hormone produced by the pancreas, plays a vital role in regulating blood glucose levels. When the body becomes resistant to insulin—a condition known as insulin resistance—it struggles to use glucose effectively, often leading to weight gain, particularly in the form of visceral fat around the abdominal area. Several factors contribute to insulin resistance.
Excess weight and obesity, especially with higher levels of abdominal fat, are strongly linked to this condition.
Physical inactivity further exacerbates the issue, as a sedentary lifestyle reduces the body’s ability to process glucose efficiently.
Aging also plays a role, with the risk of insulin resistance increasing significantly after age 45.
Cortisol: The Stress Hormone
Cortisol, often called the "stress hormone," can significantly contribute to weight gain when levels remain chronically elevated. High cortisol increases appetite, driving cravings for high-calorie, sugary, and fatty foods, which often leads to overeating.
At the same time, it encourages fat storage, particularly around the abdominal area, raising the risk of obesity and associated health problems.
Beyond these effects, elevated cortisol slows metabolism, reduces muscle mass, and decreases the body’s ability to burn calories efficiently. It also interacts with insulin by raising blood sugar levels, which can trigger insulin production and further contribute to weight gain. Managing stress is a critical part of maintaining hormonal balance and overall health.
Estrogen: The Female Hormone
Estrogen decline during menopause plays a significant role in weight gain, often leading to noticeable changes in how and where the body stores fat. Lower estrogen levels cause fat to redistribute, with an increase in abdominal fat—a pattern associated with higher health risks.
Additionally, declining estrogen contributes to muscle loss, which slows metabolism and reduces the body’s ability to burn calories efficiently.Beyond fat and muscle changes, estrogen impacts insulin sensitivity, and its reduction can lead to higher blood sugar levels, increasing the likelihood of weight gain.
Estrogen also plays a role in regulating appetite, and its decline may result in increased food intake. Combined with reduced physical activity and energy expenditure common during menopause, these factors make maintaining a healthy weight more challenging without intentional lifestyle and hormonal support.
Hypothyroidism: The Underactive Thyroid.
Hypothyroidism often sneaks in during perimenopause, making an already challenging phase of life even trickier. As estrogen and progesterone levels decline, they can throw off your thyroid’s balance, slowing your metabolism and causing symptoms like weight gain and fatigue.
It’s like your body’s engine isn’t running as efficiently as it used to, no matter how healthy your habits are.What’s more, this time of life increases the risk of autoimmune conditions like Hashimoto’s thyroiditis, which can further impact thyroid function. When your thyroid isn’t producing enough hormones, your body burns fewer calories, leaving you feeling sluggish and frustrated.
Progesterone: The Balancing Hormone
As ovulation stops during menopause, progesterone levels naturally decline, leading to noticeable changes in the body. This drop can cause bloating and water retention, resulting in temporary weight gain. When progesterone decreases more rapidly than estrogen, it can create a state of estrogen dominance, which often leads to fat accumulation around the midsection. Additionally, lower progesterone levels slow down the body's ability to burn fat efficiently, making it harder to maintain a healthy weight.
Leptin and Ghrelin: Hunger and Fullness Hormones
Leptin and ghrelin, the hormones that control hunger and fullness, can become imbalanced during perimenopause, making weight management more challenging. With leptin resistance, the body stops responding properly to leptin’s signals, leading to overeating and a slower metabolism.
At the same time, elevated levels of ghrelin—the “hunger hormone”—increase cravings, particularly for carbohydrates, further contributing to weight gain and difficulty maintaining a healthy diet.
Addressing Hormonal Imbalances
Managing weight during hormonal transitions involves addressing the root causes of these imbalances. Personalized care and support are essential to achieving relief and restoring balance
Addressing the root causes of hormonal imbalances is key to managing weight gain effectively.
If you are ready for relief and a return to balance, schedule your visit online now.
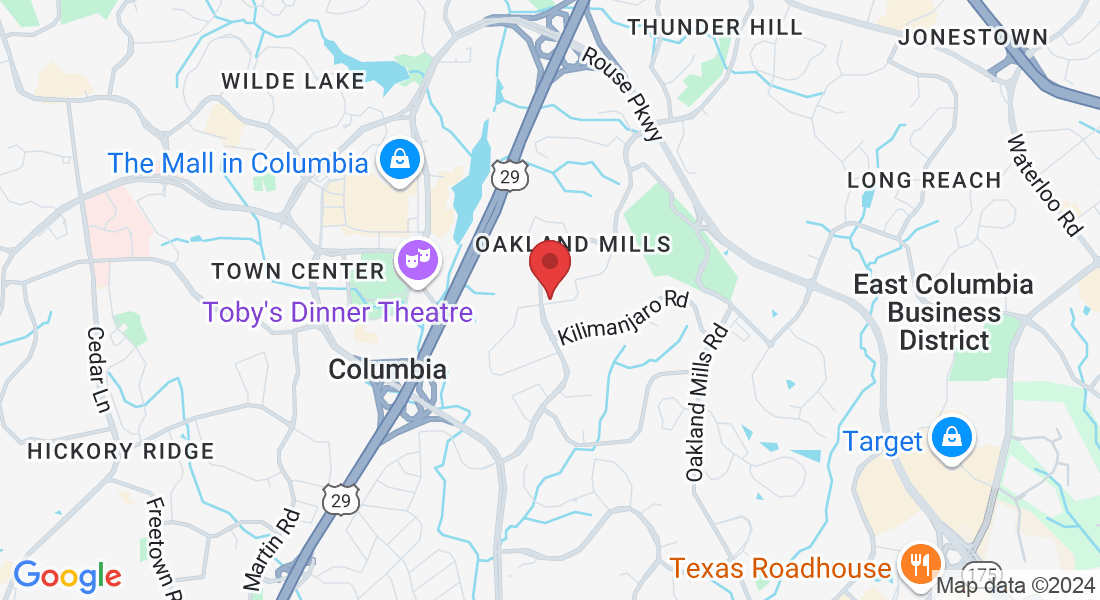
Get In Touch
Office Hours :
Monday – Friday: 8:00 am – 4:30 pm
Saturday & Sunday – Closed